Dr. Ian R. Wanless, MD, FRCPC, FAASLD
Department of Pathology, Dalhousie University, Halifax, Canada
SHORT BIOGRAPHY
Dr. Wanless is a graduate of McGill University, with post-graduate training at the University of Alberta and Cornell University Medical College, New York. After spending 28 years at the University of Toronto, he is now a Professor of Pathology at Dalhousie University and Queen Elizabeth II Health Sciences Centre in Halifax.
His research has concentrated on the pathogenesis of NASH, NRH, FNH, and the role of vascular events in the pathogenesis and regression of cirrhosis.
His studies were the first to document the role of insulin and hyperinsulinemia in human fatty liver disease, providing insight into the pathogenesis of fatty liver occurring in obesity (NASH), alcoholism, and post-jejuno-ileal bypass. He demonstrated how heterogeneity of insulin delivery to the tissues explains focal fatty change and focal fatty sparing.
His studies of the hepatic vasculature provide insights for the pathogenesis of focal nodular hyperplasia, nodular regenerative hyperplasia, non-cirrhotic portal hypertension, and cirrhosis.
Recent advances include:
- role of vascular outflow obstruction to cause parenchymal extinction followed by collapse and septum formation. Collapse of normal structural collagen causes a significant proportion of the increased collagen concentration found in cirrhosis.
- definition and mechanism of the “congestive escalator” that drives progression of disease to cirrhosis and end-stage liver failure.
- role of buds, derived from progenitor cells, to repopulate regions of collapse.
- role of congestion to inhibit bud maturation and thereby limit the ability of livers with severe cirrhosis to undergo regression.
- definition of the “nested-cone model” of hepatic vascular anatomy.
October 14, 2019
ANNOTATION OF RESEARCH ENDEAVORS
This section summarizes my most focused research activities with relevant publications clustered into 4 areas.
1. Pathogenesis of hepatic steatosis and steatohepatitis
These studies are the first to document the role of insulin in human fatty liver disease, providing insight into the pathogenesis of fatty liver of obesity (NASH), post-jejuno-ileal bypass, and alcoholic liver disease, focal fatty liver and focal fatty sparing.
- Wanless IR, Bargman J, Oreopoulos D, Vas S. Subcapsular steatonecrosis of the liver in response to peritoneal insulin delivery: A clue to the pathogenesis of steatonecrosis in obesity. Modern Pathology 1989;2:69-74.
- Wanless IR, Lentz JS. Fatty liver hepatitis (steatohepatitis) and obesity: An autopsy study with analysis of risk factors. Hepatology 1990;12:1106-1110.
- Battaglia DM, Wanless IR, Brady AP, Mackenzie RL. Intrahepatic sequestered segment of liver presenting as focal fatty change. Am J Gastroenterology 1995;90:238-239.
- Edwards L and Wanless IR. Mechanisms of liver involvement in systemic disease. Best Pract Res Clin Gastroenterol 2013;27: 471-483.
2. Pathogenesis and classification of various forms of nodular hyperplasia
These studies propose that the many different diseases having nodules of hyperplastic hepatocytes are all caused by vascular abnormalities in the liver. The various forms can be explained by the distribution of the vascular lesions. Several new varieties of nodules were described in the course of this work (telangiectatic type of FNH, multiple FNH syndrome, and focal hyperplasia with angiogenesis secondary to localized hepatic vein thrombosis (HAT) and focal hyperplasia in Budd-Chiari syndrome).
The classification (1995) formalizes this concept and is modified in a paper in 2000. This classification provides a simplified nomenclature that separates reactive from neoplastic lesions, discourages ambiguous and cumbersome terms, such as partial nodular transformation, nodular transformation, macroregenerative nodule types I and II and adenomatous hyperplasia, and defines, for the first time in human liver pathology, the dysplastic focus. Work is in progress to update this system with an international panel of hepatopathologists.
- Wanless IR, Godwin TA, Allen F, Feder A. Nodular regenerative hyperplasia of the liver in hematologic disorders: A possible response to obliterative portal venopathy. Medicine (Baltimore) 1980;59:367-379.
- Wanless IR, Solt L, Kortan P, et al. Nodular regenerative hyperplasia of the liver associated with macroglobulinemia: A clue to the pathogenesis. Am J Med 1981;70:1203-1209.
- Wanless IR, Bernier V, Seger M. Intrahepatic portal sclerosis in patients without history of liver disease: An autopsy study. Am J Pathol 1982;106: 63-70.
- Thorne C, Urowitz M, Wanless IR, Roberts E, Blendis L. Liver disease in Felty’s syndrome. Am J Med 1982;73:35-40.
- Reynolds J, Wanless IR. Nodular regenerative hyperplasia of the liver in a patient with rheumatoid arteritis. J Rheumatol 1984;11: 838-842.
- Wanless IR, Lentz JS, Roberts EA. Partial nodular transformation of the liver in an adult with persistent ductus venosus. A review with hypothesis on the pathogenesis. Arch Pathol Lab Med 1985;109:427-432.
- Wanless IR, Mawdsley C, Adams R. On the pathogenesis of focal nodular hyperplasia of the liver. Hepatology 1985;5:1194-1200.
- Wanless IR, Gryfe A. Nodular transformation of the liver in hereditary hemorrhagic telangiectasia. Arch Pathol Lab Med 1986;110: 331-335.
- Wanless IR, Albrecht S, Bilbao J, Frei JV, Heathcote EJ, Roberts EA, Chiasson D. Multiple focal nodular hyperplasia of the liver associated with vascular malformations of various organs and neoplasia of the brain: a new syndrome. Modern Pathology 1989;2:456-462.
- Wanless IR. Micronodular transformation (nodular regenerative hyperplasia) of the liver: a report of 64 cases among 2500 autopsies and a new classification of benign hepatocellular nodules. Hepatology 1990;11:787-797.
- International Working Party of World Congresses of Gastroenterology. Terminology of Nodular Lesions of the Liver. Hepatology 1995;22:983-993.
- McEntee M, Wright K, Wanless IR, DeNovo R, Shull R. Non-cirrhotic portal hypertension and nodular regenerative hyperplasia of the liver in dogs with mucopolysaccharidosis I (MPS-I). Hepatology 1998, 28:385-90.
- Wanless, IR, Terris B, Bioulac-Sage P, Balabaud C, Fléjou JF, Degott C, Belghiti J, Hemming A, Greig P. Focal Hyperplasia (FH) of liver associated with localized hepatic vein thrombosis: a lesion with some features of “focal nodular hyperplasia”. (Presented at USCAP, New Orleans, March 2000).
- Arnason T, Fleming K, Wanless IR. Peritumoural hyperplasia of the liver: a response to portal vein invasion by hypervascular neoplasms. Histopathology 2013; 62, 458–464.
3. The role of vascular disease and angiogenesis in the pathogenesis of cirrhosis
These studies describe the “The 2-hit vascular model for the pathogenesis of cirrhosis”. This model describes how 1) obliteration of the portal vein supply and the hepatic vein drainage causes obligate extinction of the supplied acinar parenchyma and 2) cirrhosis is the accumulation of many separate extinction lesions arising from discrete obliterative vascular events.
- Wanless IR, Liu J, Butany J. Role of thrombosis in the pathogenesis of congestive hepatic fibrosis (cardiac cirrhosis). Hepatology 1995;21:1232-1237.
- Wanless IR, Wong F, Blendis LM, Greig P, Heathcote EJ, Levy G. Hepatic and portal vein thrombosis in cirrhosis: possible role in development of parenchymal extinction and portal hypertension. Hepatology 1995;21:1238-1247.
- Wanless IR. Thrombosis and phlebitis in the pathogenesis of portal hypertension and cirrhosis: the 2-hit hypothesis for the pathogenesis of chronic liver disease. In Arroyo V, Bosch J, Bruguera M, Rodes J (eds). Therapy in Liver Diseases, Barcelona, Masson, 1997, pp 47-50.
- Shimamatsu K, Wanless IR. Role of ischemia in causing apoptosis, atrophy, and nodular hyperplasia in human liver. Hepatology 1997;26:343-350.
- Moreno-Merlo F, Wanless IR, Shimamatsu K, Sherman M, Greig P, Chiasson D. The role of granulomatous phlebitis and thrombosis in the pathogenesis of cirrhosis and portal hypertension in sarcoidosis. Hepatology 1997;26:554-560.
- Tanaka M, Wanless IR. Pathology of the liver in Budd-Chiari syndrome: portal vein thrombosis and the histogenesis of veno-centric cirrhosis, veno-portal cirrhosis, and large regenerative nodules. Hepatology 1998;27:488-496.
- Wanless IR, Shimamatsu K. The histogenesis of biliary cirrhosis. Mod Pathol 1999;12:169A. (Poster, USCAP, San Francisco, March 1999)
- Wanless IR. Arterialization of the liver causes baro-injury in cirrhosis and focal nodular hyperplasia (FNH) Hepatology 1999;30:571A
- Ward NL, Haninec AL, Van Slyke P, Sled JG, Sturk C, Henkelman RM, et al. Angiopoietin-1 causes reversible degradation of the portal microcirculation in mice: implications for treatment of liver disease. Am J Pathol 2004;165(3):889-99.
- Wanless IR and Huang W. Vascular disorders. In Burt AD, Portmann BC, Ferrell LD (eds). MacSween’s Pathology of the Liver, 6th edition, Churchill Livingston, Edinburgh, 2012, pp 601-643.
- Wanless IR. Physioanatomic considerations. In Schiff ER, Maddrey WC, Sorrell MF (eds). Schiff’s Diseases of the Liver, 12th edition, Wiley, Oxford, UK, 2018, pp. 73-102. (updated in 5 editions over 19 years).
- Fleming K, Wanless IR. Glutamine synthetase expression in activated hepatocyte progenitor cells and loss of hepatocellular expression in congestion and cirrhosis. Liver International, 2013: 33: 525–534
- Edwards L and Wanless IR. Mechanisms of liver involvement in systemic disease. Best Pract Res Clin Gastroenterol 2013;27: 471-483.
- Stueck, AE and Wanless IR. Hepatocyte buds derived from progenitor cells repopulate regions of parenchymal extinction in human cirrhosis. Hepatology 2015;61(5):1696-1707.
- Wanless, IR. The role of vascular injury and congestion in the pathogenesis of cirrhosis: the congestive escalator and the parenchymal extinction sequence. Curr Hepatol Reports. 2020;19(1):40-53. (PDF and video available for download, see download page)
4. The reversibility of cirrhosis
These studies demonstrate the histologic appearance of repair processes in the cirrhotic liver. Recognition of these features allows a reinterpretation of the natural history of cirrhosis, incomplete septal cirrhosis, and various types of noncirrhotic portal hypertension such as idiopathic portal hypertension. The major conclusion is that cirrhosis is in a constant state of regression towards normal. In most chronic diseases, this process of regression is interrupted by periods of activity that worsen the state of fibrosis. Currently, work is in progress to define the factors that prevent regression of some fibrous septa and thus prevent regression in many patients.
- Nakashima E, Kage M, Wanless IR. Idiopathic portal hypertension: Histologic evidence that some cases may be regressed cirrhosis with portal vein thrombosis. Hepatology 1999;30:218A. (Poster presented at AASLD, Dallas, Nov 1999.)
- Wanless IR, Nakashima E, Sherman M. Regression of human cirrhosis: morphologic features and the genesis of incomplete septal cirrhosis. Arch Pathol Lab Med 2000 124:1599-607.
- Wanless IR. Regression of human cirrhosis: In Reply. Arch Pathol Lab Med 2000;124:1592-3.
- Ward NL, Haninec AL, Van Slyke P, Sled JG, Sturk C, Henkelman RM, et al. Angiopoietin-1 causes reversible degradation of the portal microcirculation in mice: implications for treatment of liver disease. Am J Pathol 2004;165(3):889-99.
- Nakashima E, Wanless IR. Most non-cirrhotic livers with hepatocellular carcinoma (HCC) have evidence of fibrosis or regressed cirrhosis: implications for the pathogenesis of HCC. Hepatology 1999;30:257A. (Poster presented at AASLD, Dallas, Nov 1999.)
- Wanless IR and Huang W. Vascular disorders. In Burt AD, Portmann BC, Ferrell LD (eds). MacSween’s Pathology of the Liver, 6th edition, Churchill Livingston, Edinburgh, 2012, 601-643.
- Stueck, AE and Wanless IR. Hepatocyte buds derived from progenitor cells repopulate regions of parenchymal extinction in human cirrhosis. Hepatology 2015;61(5):1696-707.
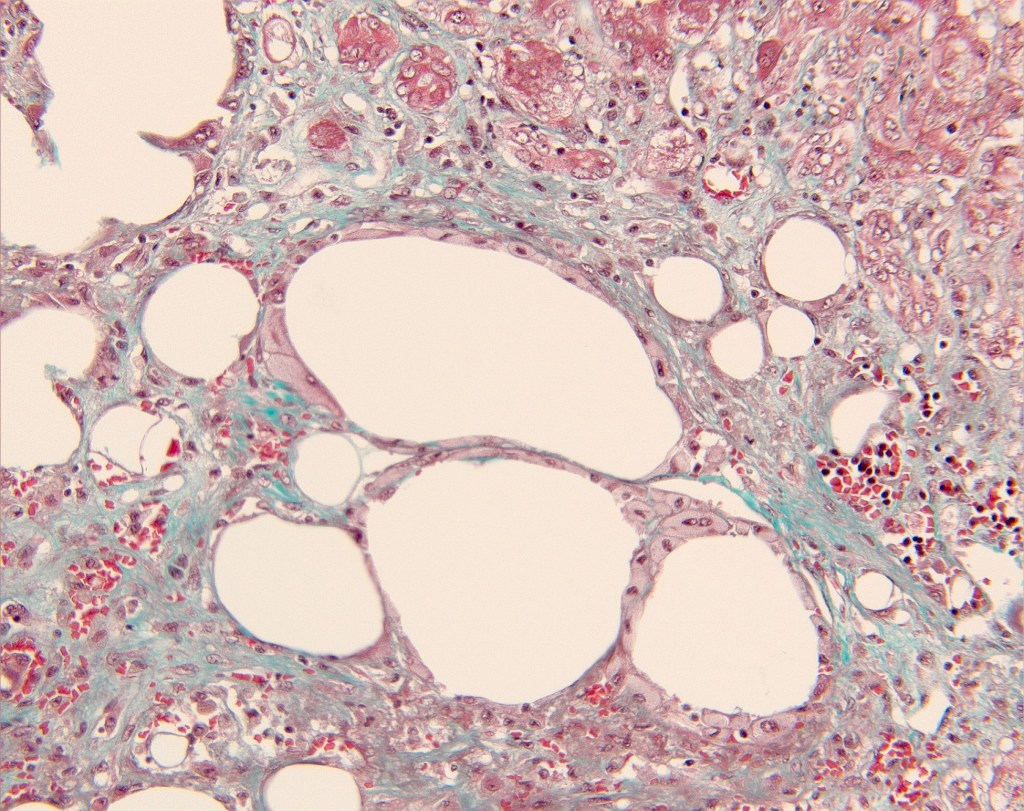
lipopeliosis